2009 - 2013 Gwen Dewar, Ph.D., all rights reserved
Bed sharing in cross-cultural perspective
Throughout human history, babies and mothers have slept together,
often sharing a sleep surface (Konner 1981). Is this a safe
arrangement?
The answer depends on the details. The typical, Western-style bed
is not a safe place for babies to sleep. And there are people whose
habits make them dangerous bed partners.
But some sleeping arrangements are much safer than others. For
instance, there may be little or no added risk associated with shared
sleep as it has been practiced in traditional Japan. In fact, it might
even be
safer than solitary sleep.
More generally, bed sharing seems to be pretty safe for older
babies. If you read the scientific and medical literature, the
controversy about bed sharing safety primarily concerns babies less than
20 weeks old, and the most recent meta-analysis of published studies
found no evidence of increased risk for babies over 3 months of age
(Carpenter et al 2013).
Here I describe the specific circumstances that are linked with
higher rates of mortality among young babies. In addition, I describe
the arguments for and against sharing a bed. Last, I review what
researchers agree about.
As noted below, most researchers agree that young babies should
sleep in the same room where their parents sleep. The point of
disagreement is whether parents should be advised against sharing their
beds.
Some researchers think that the safest arrangement involves
cosleeping without sharing the same bed--i.e., placing a young infant in
a crib or “side car" that is within arm’s reach of his parent. But it's
not yet clear if a stringent approach to sharing a sleep surface -- an
approach that eliminates the hazards posed by Western beds and sleep
habits -- is linked with any elevated risk.
Understanding the hazards of bed sharing with infants
Several organizations have issued recommendations against bed sharing
for infants (e.g., the American Academy of Pediatrics). These
organizations base their recommendations on Western studies linking bed
sharing with increased
SIDS
rates for babies under 20 weeks old. In addition, babies who sleep in
traditional, Western-style adult beds may be at greater risk of
accidental injury or death.
Why? Much of the risk is associated with specific cultural practices.
Smoking and the risk of SIDS
There is something about smoking that makes bed sharing very
dangerous. Studies suggest that the odds of SIDS, or sudden infant death
syndrome, are much greater -- 16 to 100 times greater -- for babies who
bed share with a mother or other adult who smokes. This pertains to
both prenatal exposure--i.e., babies whose mothers smoked during
pregnancy--and to postnatal exposure to household smoke (Horsley et al
2007; Carpenter et al 2013).
Why the link? That’s not yet clear. Research suggests that babies
who are exposed to smoke have more difficulty arousing from sleep,
perhaps because smoke exposure changes the serotonin pathways of the
brain (Kinney 2009). And when babies having difficulty arousing, they
are at increased risk for SIDS.
But regardless of the mechanism, there is a consensus that
smokers shouldn’t bed share, and that smoking can explain much of the
elevated SIDS risk associated with shared sleep.
In some studies, the risk of bed sharing became statistically
insignificant after researchers controlled for maternal smoking (e.g.,
Scragg et al 1993; Blair et al 1999; McGarvey et al 2003). However, more
recent studies suggest an elevated risk still exists among nonsmokers
in Western populations (Carpenter et al 2013).
Dangerous sleeping surfaces
Sofas, chairs, and waterbeds are very dangerous places for babies to
sleep. Indeed, an analysis of SIDS cases in Scotland found that the risk
of mortality increased 60-fold for babies cosleeping on sofas (Tappin
et al 2005).
Compared to a sofa, chair, or water bed, a conventional bed might seem less hazardous. But the typical Western bed wasn’t designed for babies, and it presents several dangers (Nakamura et al 1999; Kemp et al 2000).
• Western beds may include pillows, loose bedding, heavy
blankets, duvets, or soft mattresses--all hazards for accidental
suffocation, re-breathing asphyxia, and SIDS.
• Babies can get trapped in the spaces between a mattress and a wall, headboard, or footboard.
• Bed rails pose a strangulation hazard.
• Western beds are elevated from the floor, creating a falling hazard.
• Even a bed sheet or light blanket poses a risk if it can cover a baby’s face
This last point shouldn’t be overlooked, because research
suggests that any kind of covering--even a thin bed sheet--can make it
harder for babies to arouse from sleep (Franco et al 2002).
This suggests that the sleeping environment is safer when parents
and babies sleep without any coverings at all. When people sleep under
sheets or blankets, these coverings tend to end up over the baby's
face.
A study mother-infant pairs in New Zealand found that bed sharing infants were far more likely than were solitary sleepers to spend time with blankets covering their noses, faces, or entire heads (Baddock et al 2006).
Unsafe sleeping companions
Let's imagine a sleeping surface that is firm and free of known
hazards--like loose bedding and bed rails. What risks are posed by the presence of another person in bed?
Are babies at risk of being smothered?
Perhaps a parent's biggest fear is overlaying--i.e., a baby getting
smothered because somebody accidentally rolls onto him during sleep.
What percentage of bed sharing incidents end in this horrifying way?
Such accidents have been documented in the United States and
elsewhere (e.g., Nakamura et al 1999; Kemp et al 2000; Shapiro-Medonza
et al 2009). But because we lack information about the prevalence of bed
sharing, it’s hard to quantify the risk.
There is evidence regarding the frequency of adults rolling over.
In a study by Sally Baddock and colleagues, 40 mother-infant
pairs were videotaped and monitored as they slept together in their own
homes on two consecutive nights. The researchers observed no instances
in which the mother obstructed the baby’s airways. Nor did the babies
experience any unusual changes in oxygen level or body temperature
(Baddock et al 2006). Such findings are supported by the experiences of
James McKenna, who has conducted decades of
laboratory research on mother-infant bed-sharing.
Of course, this doesn’t mean that it never happens. A recent
survey of bed-sharing mothers in Canada found that 13% of the
respondents recalled at least one episode in which someone (e.g., the
mother or father) had rolled onto or part way onto their infants (Ateah
and Hamelin 2008).
In these cases, none of the infants were hurt. The sleeper was awakened before any injury occurred.
That’s probably normal--at least when the sleeper is a healthy
mother unimpaired by drugs, alcohol or exhaustion. As James McKenna has
argued, mothers and infants have slept together for millions of years.
Natural selection would have favored traits that keep mothers attuned to
their babies during sleep.
And research suggests that mothers who routinely bed-share are light sleepers.
In a laboratory study, mothers experienced 30% more arousals when
they slept with their infants (Mosko et al 1997a). And mother-infant
pairs tend to sleep in synchrony, with more than 70% of their arousals
overlapping (Mosko et al 1997b). Moreover, mothers who bed-share check
on their babies more frequently during the night. In Baddock’s study,
bed sharing mothers checked on their babies a median of 11 times. For
mothers sleeping in separate beds, the median was 4 (Baddock et al
2006).
Who should never bed share: High-risk groups
Presumably, at least some of the incidents reported in the Canadian
study could have ended badly if people on the scene had been less alert.
And indeed, case studies of SIDS and accidental death have linked
higher mortality rates with certain kinds of bed-sharers.
For example, there is evidence that sharing a sleep surface is
more dangerous for babies of low birth weight (low for gestational age
or less than 2500 grams - McGarvey et al 2006).
Researchers also agree that children should not sleep with young babies.
In addition,
• The risk of infant death is greatly increased when bed
sharing parents have consumed alcohol or any other drugs or medications
that impair alertness and judgment (Carpenter et al 2004; Blair et
al 1999; McGarvey et al 2006). In the most recent meta-analysis of
published studies, Robert Carpenter and colleagues found that the risk
of SIDS increases dramatically for young babies when their mothers have
consumed 2 units or more of alcohol in the previous 24 hours. For
example, the odds for 2-week-babies increase almost 90-fold. And the
increased risk of death for babies sharing beds with drug-using mothers
was "unquantifiably large" (Carpenter et al 2013).
• Sleeping together is also more dangerous when parents are very tired (Blair
et al 1999). Presumably, people sleep more deeply when they are
overtired and might be less likely to awaken when their baby is in
danger.
• It’s also about how many people are in the bed. In an
analysis of SIDS deaths in Chicago, researchers controlled for various
SIDS risk factors, including maternal smoking, soft sleep surface,
pillow use, prone sleep position, and pacifier use. They found that
sharing a bed with two other people was linked with a significant
increase in SIDS risk. And the risk of SIDS increased dramatically if
babies shared a bed with three or more people. By contrast, the
researchers observed no increased SIDS risk for babies who shared their
beds with just one person--their mothers (Hauck and Herman 2006).
Other risk factors
Bed sharing mortality has been linked with markers of lower
socioeconomic status (SES), including overcrowded households, adolescent
mothers, economic deprivation, and low levels of maternal education
(e.g., Carpenter et al 2004; Fleming 2006; Ostfeld et al 2006).
Why? Lower SES is linked with higher rates of mortality in
general, as well as higher rates of risky practices, like smoking. It
also seems likely that SES is correlated with other conditions of the
shared sleeping environment, like air quality and the condition of the
mattress.
In any case, links between mortality and socioeconomic factors
seem to underscore the point: The risks of shared sleep depend on the
context.
Babies with multiple risk factors are especially vulnerable
In their recent meta-analysis of European case-control studies,
Robert Carpenter and his colleagues (2013) note that risk factors don't
just add up, they multiply. As as result, "infants with multiple risk
factors are likely to be at a far greater risk than is generally
supposed."
For example, the researchers estimate that a baby who shares a bed
with two smoking parents has 65 times the risk of SIDS. But if this baby
is also bottle-fed (with 1.5 times the risk), male (1.6 times), and of
low birth weight (4.2 times), his overall risk is 655 times greater than
it would be if he didn't bed share.
What about sleeping on a safe surface with a healthy, sober, non-smoking parent?
As of 2013, no one yet has demonstrated that keeping a baby in a crib
or cot is any less hazardous than this mother-infant sleeping
scenario:
• The sleeping surface is a firm mattress or mat pushed away from the wall and all other furniture
• There is no headboard, footboard, or railing attached to the bed
• The baby is placed on his back and his face is uncovered.
• There are no bed covers (neither blankets, duvets, nor top
sheets), no soft toys and no dangerous bedding (e.g., pillows) near the
baby.
• Care is taken to prevent the baby from overheating (i.e., the
room is a comfortable temperature and the baby isn’t overdressed)
• There are no draperies, blinds, or cords nearby that the baby could get tangled in
• Neither mother nor infant is wearing anything could cover the
baby’s face, get tangled around the baby’s neck, or constitute a choking
hazard
• The baby can’t hurt himself by falling out of bed. For example,
if the bed is elevated from the ground, the baby is protected from
falling out by being placed between the mother and a safe barrier, like
the Humanity Family Bed Cosleeping Pad.
• The mother is a nonsmoker and is unimpaired by alcohol, drugs, or exhaustion
• The mother doesn’t suffer from medical conditions that render her a “heavy" sleeper or a “restless" sleeper
• The mother is the only person sharing the sleeping surface with the baby
This might sound like a lot of stipulations. But these stipulations
may be life-saving, and they reflect the traditional sleeping conditions
found in places like Japan, where SIDS rates are low (Nelson et al
2001; Hauck and Tanabe 2008).
In fact, this scenario--which I’ll call the “primal co-sleeping
scenario"--has probably been the most common infant sleeping arrangement
in human history.
Does this mean that the “primal co-sleeping scenario" is risk-free?
No. As noted above, we lack studies regarding the safety of this
style of co-sleeping. But until such studies are conducted, it's
reasonable to assume that eliminating known hazards from the sleep
environment will reduce risk to the baby.
For example, in one study of SIDS cases, the risk of sharing a bed
became statistically insignificant after researchers controlled for the
effects of recent maternal alcohol consumption, infant duvet use,
overcrowding, and parental tiredness (Blair 2006).
And, as mentioned above, another study found no elevated SIDS
risk for babies who shared a bed with their mothers only (Hauck and
Herman 2006).
As researcher Peter Blair has noted, “It may not be bed-sharing per se, but the particular circumstances in which bed sharing occurs that is dangerous" (Blair 2006).
What’s the safest place for young babies?
Recommendations against bed sharing
In their 2005 policy statement, the American Academy of Pediatrics (AAP) Task Force on Sudden Infant Death Syndrome wrote
"...bed sharing, as practiced in the United States and other Western countries, is more hazardous than the infant sleeping on a separate sleep surface"
(AAP Task Force on Sudden Infant Death Syndrome 2005; emphasis mine).
As a result, the Task Force says, parents should avoid bed
sharing. Instead, a baby can sleep in a crib or cot placed alongside the
parent’s bed.
The Task Force based this recommendation on the European
Concerted Actions on SIDS (“ECAS") study, an analysis of sudden
unexplained infant death cases reported in 20 different regions of
Europe (Carpenter et al 2004). According to the ECAS data, bed sharing
posed a significant risk for babies under 12 weeks of age, even for
nonsmokers (Carpenter 2006). The SIDS risk was lowest for babies who
slept in the same room as their parents--but in their own crib or cot.
More recently, Robert Carpenter and his colleagues performed
another analysis of five European case-control studies (including the
original ECAS) published in the 1990s.
Just as in the original ECAS study, the researchers didn’t
control for the firmness of the mattress or the identity and number of
people sharing a bed. Nor did researchers test the scrupulous “primal
co-sleeping scenario" outlined above. Their analysis concerned shared
sleep as it is typically practiced by Europeans – soft mattresses,
loose bedding, and all.
But they did calculate the dangers for young babies who are
usually considered low risk for SIDS – babies with parents who don’t, as
a habit, smoke or drink – and they controlled for other factors like
birth weight and breastfeeding.
Under these conditions, infant death was, on average, five times
more likely among babies who bed-shared during the first 3 months
postpartum (Carpenter et al 2013). And for lead author Carpenter, the
implications are clear. As he told interviewer Salynn Boyles,
"For the first 3 months of life, babies should not sleep with
their parents. Period. After that, if the parents don't smoke, it might
be OK" (Boyles 2013).
Are such recommendations too sweeping? People concerned with broad, population-wide trends might say no.
The argument for general recommendations against bed sharing
True, these studies didn't control for the number and identity of
people sharing the bed, nor did they address key risk factors
associated with Western beds (Carpenter et al 2005; Carpenter 2006;
personal communication 2008).
And on theoretical grounds, it isn't clear why bed sharing per se (as opposed to the particular circumstances of bed sharing) might put babies at higher risk of SIDS.
But the medical community didn’t wait to discover why
babies who slept on their stomachs were more likely to die of SIDS.
Once the link was established, parents were advised to place babies on
their backs. And this approach paid off: As the “Back to Sleep" campaign
spread, SIDS rates fell.
Moreover, even if there were no SIDS risk, there is still the
risk of accidents. And the most certain way to prevent bed sharing
accidents is to stop people from bed sharing.
So some people think it makes sense to avoid bed sharing altogether--at least for infants in the first few months after birth.
However, even putting aside objections about missing data, this
argument doesn’t take into account the potential benefits of sharing a
bed.
The benefits of bed sharing
Sleep, breastfeeding, bonding, and stress management
Sleeping together makes nocturnal breastfeeding less disruptive, and
mothers who bed-share and breastfeed may get more sleep than do mothers
who bottle-feed (Quillan and Glenn 2004).
This might explain why mothers who sleep with their babies
• spend more time breastfeeding at night (McKenna et al 1999; Gettler and McKenna 2011), and
• are more likely to continue breastfeeding over the long-term (Horsley et al 2007)
So shared sleep may benefit babies by increasing the duration of breastfeeding.
Emotional comfort and bonding
Bed sharing appears to have emotional benefits, too. Many parents
feel that bed sharing strengthens their emotional bonds with their
babies (McKenna and Volpe 2007).
Do the babies feel better? Experimental evidence suggests that
they might. For example, sleeping together promotes skin-to-skin
contact, and studies indicate that skin-to-skin contact—with or without
breastfeeding--reduces physiological stress in infants (Gray et al 2000;
Gray et al 2002).
Safety and protection from SIDS
Sleeping together permits parents to closely monitor their babies
throughout the night. For instance, a parent may be more likely to
notice if her baby has adopted a dangerous sleep position or has become
ill. Indeed, one survey collected anecdotal accounts from parents who
believed that bed sharing may have saved their babies lives (McKenna and
Volpe 2007). Many of these parents reported that sharing a bed allowed
them to identify and immediately intervene when their babies suffered
respiratory crises.
Bed sharing might also have a protective effect against SIDS.
That’s because babies who bed share experience more frequent arousals
from sleep, and frequent arousals reduce the risk of SIDS (Mosko et al
1997; Mao et al 2004; McKenna and McDade 2005).
Bed sharing may protect babies indirectly, too. As noted above,
bed sharing might encourage mothers to breastfeed, and babies who are
breastfed have a reduced risk of being victimized by SIDS (Venneman et
al 2009). Although it’s not yet clear why, one hypothesis is that
breastfeeding protects babies via benefits to the immune system.
According to this idea, breastfed babies are less likely to succumb to
pathogens that can trigger life-threatening respiratory events.
A crucial tool for coping with high-need babies?
I think it’s important to recognize that some young babies have a
very difficult time sleeping apart from their parents. For these
so-called “fussy" or “high need" babies, the standard pediatric
recommendations and folk remedies don’t seem to work (Sears and Sears
1996). The baby doesn’t fall asleep or stay asleep unless she is in
close contact with a caregiver. Such babies may demand very frequent
feedings, too. For the minority of parents who cope with high-need
babies, sleeping together may seem like the only practical way for a
family to get quality sleep.
Weighing the risks and benefits
For those parents who want to practice bed sharing, there may be quite a bit at stake.
Rather than abandon bed sharing, such parents may choose to
modify their sleeping environment, eliminate known hazards, and practice
the safest form of bed sharing possible.
As noted above, current studies address bed sharing “as practiced
in the United States and other Western countries" (AAP Task Force on
Sudden Infant Death Syndrome 2005). At present, it’s not known if the
net risks of the “primal sleep scenario" are any greater than the net
risks of using a cot or crib.
But it’s important to recognize how very far the typical Western,
adult sleeping environment is from the primal sleep scenario outlined
above. Accidental bed sharing deaths may be on the rise in the United
States, particularly among socially and economically disadvantaged
populations (Shapiro-Mendoza 2009). Some researchers speculate that this
is because hazardous forms of bed sharing are becoming more common.
So we shouldn’t be complacent about these hazards. For parents
living in the West, low-risk bed sharing may require some dramatic
changes to their bedrooms and sleep routines.
Alternatively, parents may opt for other co-sleeping
alternatives, like attaching an especially-designed baby “side car" to
the side of the parental bed. One example is the Arm’s Reach cosleeper, a
product endorsed by pediatrician William Sears and anthropologist James
McKenna. As its name suggests, it permits parents to keep babies within
arm’s reach—-something that just about every researcher agrees is a
good idea.
The bottom line?
Researchers on both sides of the debate agree that
• Accidents happen. Although we lack information to quantify the
risk, it’s clear that some babies have died in accidents on adult beds.
• Babies shouldn’t sleep on sofas, armchairs, or waterbeds
• SIDS rates are higher for babies who bed share if they were born preterm or were born small for their gestational age
• Babies shouldn’t share beds with adults who smoke or who are impaired by drugs, alcohol, or exhaustion
• Children and young babies shouldn’t sleep in the same bed
• Babies shouldn’t be left alone in adult beds
• Babies shouldn’t sleep in beds that include features known to
be hazardous--like soft mattresses, loose bedding, and the entrapment
hazards named above. Even a bed sheet may pose a risk.
Researchers also agree that
• It’s a good idea for young babies to sleep in the same room as their parent(s)
• The most recent meta-analysis of five case-control studies of
European populations found a five-fold increased risk for young babies
(< 3 months old) who bed share--even when the mothers were nonsmokers
and avoided alcohol.
• Such studies haven’t controlled for all possible confounding variables, especially the many hazards posed by Western beds
Why is there a link between bed sharing and SIDs in these studies?
Future research--randomized, controlled, prospective studies--will help us answer this question.
Meanwhile, there is controversy about how medical professionals
should advise parents. Should official recommendations discourage
parents from all forms of bed sharing? Or should parents be provided
with information about the specific circumstances known to make bed
sharing risky?
Given the mission of this website, you can probably guess my own
position. According to Peter Blair, the current practice in England is
to avoid a “one size fits all" piece of advice. Instead, “parents are
given the information as it is" (Blair 2006).
Sounds like a good idea to me.
References
American Academy of Pediatrics Task Force on Sudden Infant Death
Syndrome. 2005. The changing concept of sudden infant death syndrome:
diagnostic coding shifts, controversies regarding the sleeping
environment, and new variables to consider in reducing risk. Pediatrics.
116(5):1245-55.
Ateah CA and Hamelin KJ. 2008. Maternal bedsharing practices,
experiences, and awareness of risks. J Obstet Gynecol Neonatal Nurs.
37(3):274-81.
Baddock SA, Galland BC, Bolton DP, Williams SM, and Taylor BJ.
2006. Differences in infant and parent behaviors during routine bed
sharing compared with cot sleeping in the home setting. Pediatrics
117(5):1599-607.
Blair PS. 2006. Sudden infant death syndrome epidemiology and bed sharing. Peadiatr Child Health 11 (Suppl A): 29A-31A.
Blair PS, Sidebotham P, Berry PJ, Evans M, and Fleming PJ. 2006.
Major epidemiological changes in sudden infant death syndrome: A 20-year
population-based study in the UK. Lancet 367: 314-319.
Blair PS, Fleming PJ, Smith IJ, et al. 1999. Babies sleeping with
parents: Case-control study of factors influencing the risk of the
sudden infant death syndrome. CEDSI SUDI research group. BMJ 319:
1457-1462.
Boyles S. "Any bed-sharing puts baby at risk for SIDS." 2013, May
20. Medpage Today. Web article at
http://www.medpagetoday.com/Pediatrics/Parenting/39283 accessed on
5/23/2013.
Carpenter RG, Irgens LM, Blair PS, England PD, Fleming P, Huber
J, Jorch G, and Schreuder P. 2004. Sudden unexplained infant death in 20
regions in Europe: case control study. Lancet 363(9404): 185-191.
Carpenter RC. 2006. The hazards of bedsharing. Peadiatr Child Health 11 (Suppl A): 24A-28A.
Franco P, Lipshultz W, Valente F, Adams S, Scaillet S, and Kahn
A. 2002. Decreased arousals in infants who sleep with the face covered
by bedclothes. Pediatrics 109: 1112-1117.
Getter L and McKenna J. 2011. Evolutionary Perspectives on
Mother–Infant Sleep Proximity and Breastfeeding in a Laboratory Setting.
Am J Phys Anthropol. 144(3): 454–462.
Gray L, Miller LW, Philipp BL, Blass EM. 2002. Breastfeeding is analgesic in healthy newborns. Pediatrics 109: 590-593.
Gray L, Watt L, Blass EM. Skin-to-skin contact is analgesic in healthy newborns. Pediatrics 105(1).
Hauck FR and Herman SM. 2006. Bed sharing and sudden infant death
syndrome in a largely African-American population. Peadiatr Child
Health 11 (Suppl A): 16A-18A.
Hauck FR and Tanabe KO. 2008. International trends in sudden
infant death syndrome: stabilization of rates requires further action.
Pediatrics 122(3):660-6.
Horsley T, Clifford T, Barrowman N, Bennett S, Yazdi F, Sampson
M, Moher D, Dingwall O, Schachter H, and Côté A. 2007. Benefits and
Harms Associated With the Practice of Bed Sharing. Arch Pediatr Adolesc
Med. 161(3):237-45.
Kemp JS, Unger B, Wilkins D, Psara RM, Ledbetter TL, Graham MA,
Case M, Thach BT. 2000. Unsafe sleep practices and an analysis of
bedsharing among infants dying suddenly and unexpectedly: results of a
four-year, population-based, death-scene investigation study of sudden
infant death syndrome and related deaths. Pediatrics 106(3):E41.
Kinney HC. 2009. Brainstem mechanisms underlying the sudden
infant death syndrome: evidence from human pathologic studies. Dev
Psychobiol. 51(3):223-33.
Konner M. 1981. Evolution of human behavior development. In RH
Monroe, R Monroe and JM Whiting (eds): Handbook of cross-cultural
development. New York: Garland STPM Press.
Mao A, Burnham MM, Goodlin-Jones BL, Gaylor EE, and Anders TF.
2004. A comparison of the sleep-wake patterns of co-sleeping and
solitary infants. Child Psychiatry and Human Development 32(2): 95-105.
McGarvey C, McDonnell, Hamilton K, O’Regan M, and Matthews T.
2006. Bed sharing and sudden infant death syndrome: Irish case-control
study. Peadiatr Child Health 11 (Suppl A): 19A-21A.
McGarvey C, McDonnell M, Chong A, O’Regan M and Matthews T. 2003.
Factor relating to the infant’s last sleeping environment in sudden
infant death syndrome in the Republic of Ireland. Arch Dis Child 88:
1058-1064.
McKenna JJ and McDade T. 2005. Why babies should never sleep
alone: A review of the co-sleeping controversy in relation to SIDS,
bedsharing and breast feeding. Paediatric Respiratory Reviews (2005) 6,
134–152.
Mosko S, Richard C, and McKenna J. 1997. Maternal sleep and arousals during bedsharing with infants. Sleep 20(2): 142-150a.
Mosko S, Richard C, McKenna J. 1997b. Infant arousals during
mother-infant bed sharing: implications for infant sleep and sudden
infant death syndrome research. Pediatrics. 100(5):841-9.
Nakamura S, Wind M, and Danello MA. 1999. Review of hazards
associated with children placed in adult beds. Arch Pediatr Adolesc
Med.153(10):1019-23.
Nelson E, Taylor B, Jenik A, Vance J, Walmsley K, Pollard K, et
al. 2001. International child care practices study: infant sleeping
environment. Early human development 62: 43-55.
Ostfeld BM, Perl H, Esposito L, Hempstead K, Hinnen R, Sandler A,
Goldblatt Pearson, Hegyi T. 2006. Sleep environment, positional,
lifestyle, and demographic characteristics associated with bed sharing
in sudden infant death syndrome cases: A population-based study.
Pediatrics 118(5): 2051-2059.
Quillin SI and Glenn LL. 2004. Interaction between feeding method
and co-sleeping on maternal-newborn sleep. J Obstet gynecol Neonatal
Nurs 33(5): 580-588.
Scragg R, Mitchell EA, Taylor BJ, and the New Zealand Cot Death
Study Group. 1993. Bed sharing, smoking, and alcohol in the sudden
infant death syndrome. BMJ 307: 1312-1318.
Sears W and Sears M. 1996. The fussy baby book: Parenting your
high-need child from birth to age five. New York: Little, Brown and
Company.
Shapiro-Mendoza CK, Kimball M, Tomashek KM, Anderson RN, and
Blanding S. 2009. US infant mortality trends attributable to accidental
suffocation and strangulation in bed from 1984 through 2004: are rates
increasing? Pediatrics. 123(2):533-9.
Tappin D, Ecob R, and Brooke H. 2005. Bedsharing, roomsharing,
and sudden infant death syndrome in Scotland: a case-control study. J
Pediatr. 147(1):32-7.
Vennemann MM, Bajanowski T, Brinkmann B, Jorch G, Yücesan K,
Sauerland C, Mitchell EA and GeSID Study Group. 2009. Does breastfeeding
reduce the risk of sudden infant death syndrome? Pediatrics.
123(3):e406-10.
Content last modified 5/13
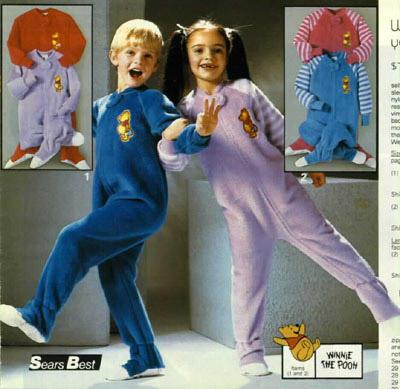
 KellyNovember 4, 2011 at 8:07 PMNow if only someone would invent a sleeper with a belly button hole! My son is a belly-button twirler, and we haven't been able to do any one-pieces of any kind since he was tiny as a result. No onesies! No sleepers! MUST have belly button access.Reply
KellyNovember 4, 2011 at 8:07 PMNow if only someone would invent a sleeper with a belly button hole! My son is a belly-button twirler, and we haven't been able to do any one-pieces of any kind since he was tiny as a result. No onesies! No sleepers! MUST have belly button access.Reply I'm at a loss as to why PJs disappear after 5T. My 8 y.o. still needs PJs. It is close to impossible to find, especially not made in China & loaded with licensed characters. Yay for everyone with littles who can buy these wonderful jammies. I am super jealous!Reply
I'm at a loss as to why PJs disappear after 5T. My 8 y.o. still needs PJs. It is close to impossible to find, especially not made in China & loaded with licensed characters. Yay for everyone with littles who can buy these wonderful jammies. I am super jealous!Reply We're looking into ideas for older kids. As Snug Organics grows we'd love to be able to offer larger sizes. I think as kids grow older they tend to keep blankets on and don't need such warm sleepwear. 100% cotton long johns seem to be the only organic option for my older son. We'll be working on it!Reply
We're looking into ideas for older kids. As Snug Organics grows we'd love to be able to offer larger sizes. I think as kids grow older they tend to keep blankets on and don't need such warm sleepwear. 100% cotton long johns seem to be the only organic option for my older son. We'll be working on it!Reply Wow, they are lovely. Pretty pricey, though. I'm in New Zealand and on the search for organic pjs but am still looking for an option a bit closer to home :)Reply
Wow, they are lovely. Pretty pricey, though. I'm in New Zealand and on the search for organic pjs but am still looking for an option a bit closer to home :)Reply My baby also loves fuzzy pj's I think every baby loves it.Reply
My baby also loves fuzzy pj's I think every baby loves it.Reply I'm looking for this type of pajama but need the footie feature also (socks always come off in the crib). Are there any companies who sell warm footie pajamas without flame retardants? The ones from Carter's are not warm enough and fleece always seems to have flame retardants.Reply
I'm looking for this type of pajama but need the footie feature also (socks always come off in the crib). Are there any companies who sell warm footie pajamas without flame retardants? The ones from Carter's are not warm enough and fleece always seems to have flame retardants.Reply